COVID-19 ushers in age of digital, flexible EU pharmaceutical regulation

The pandemic that has swept over the world in 2020 has caused huge disruption to the European pharmaceutical industry's regulatory procedures and supply chain management. But the crisis has also provided a platform for a learning process for the system to be more flexible, not least in terms of advancing a more digitized approach...
The coronavirus pandemic has changed how drugs are made and regulated in the European Union (EU) and significantly impacted pharmaceutical manufacturing supply chains.
The SARS-CoV-2 virus was first detected in Wuhan, China in December. While there are some critics, the consensus (1) is that the Chinese Government’s response – early reporting and situation monitoring, large-scale surveillance, citizen lockdowns and preparation of medical facilities and supplies - were all successful in reducing the epidemic in China.
However, the suspension of manufacturing by the country’s fine chemicals industry disrupted global pharmaceutical supply chains, according to Zhengxi Danard of Voisin Consulting Life Sciences.
“The supply chain of APIs, excipients, reagents and finished drug products have been impacted insofar as plants in China could no longer provide these starting materials and drug substances or intermediate products to the industry. In a few days, European stocks of some APIs and drug products melted like snow in springtime,” she says. “The pharma industry had to face both shortage of Chinese materials, including small equipment, like chromatography columns or simple laboratory reagents.”
Increased demand for intensive care products has been a particular problem, according to Danard.
“We witnessed that pharma companies faced production challenges, especially those manufacturing drug products typically used in ICU. Indeed Hospitals & EU governments, notably, have ordered a huge quantity of products to make sure they will have sufficient stock to meet the high demand.”
Inspection disruption
Manufacturing facility inspections have also been significantly disrupted.
The European Medicines Agency does not conduct inspections itself, rather it requests that inspections be carried out by national authorities in the EU Member States; so it is well placed to assess the impact of the pandemic.
EMA spokeswoman Beatriz Romero says that due to the travelling restrictions imposed in several countries, the number of overall inspections carried out physically for GCP and GMP have been reduced.
To address this, the European Commission, EMA and national competent authorities have agreed measures to reduce disruption, she adds.
“A harmonised procedure for performing distant assessment/remote inspection of manufacturing sites has been agreed...and the national inspectorates have this additional tool to be used if and when a site cannot be physically reached." - Beatriz Romero, European Medicines Agency
“The mitigation measures have been taken to ensure the continued availability of medicines, whilst making sure that good practice standards are being adhered to,” she says.
The measures – detailed in a Q&A document (2) – include extending the validity of GMP certificates and time-limited manufacturing and import authorisations until 2021, with the option of remote audits as needed.
According to Romero, “a harmonised procedure for performing distant assessment/remote inspection of manufacturing sites has been agreed by the GMDP IWG (Inspectors Working Group), and the national inspectorates have this additional tool to be used if and when a site cannot be physically reached. This is particularly useful for the conduction of those inspections which are necessary in order to finalise new applications.”
Clinical trials
In addition, the pandemic has severely disrupted clinical trials across the EU – with good clinical practice (GCP) inspections – being a particular challenge.
GCP inspections are designed to ensure the rights, safety, and wellbeing of trial participants are protected, and that the clinical study data used to support marketing authorisations of medicinal products in the EU / EEA are accurate and reliable.
According to Romero, the EMA’s working group has sought to minimize the impact on clinical research by making assessments at distance.
“Given the challenges in performing on-site inspections during this crisis period and in order to enable the continuity of GCP inspections requested by the Committee for Medicinal Products for Human Use (CHMP), the GCP Inspectors Working Group (GCP IWG) adopted a guidance on conducting GCP inspections remotely during the COVID-19 pandemic.”
The remote assessment measures were published in May (3).
For Zhengxi Danard from Voisin Consulting Life Sciences, the results of efforts to support clinical trials were mixed.
“Agencies were more tolerant on a number of aspects, for example the increase in protocol deviations but it was also quite challenging to identify and follow the new requirements in each EU country, which were updated very regularly,” She says. “Agencies were also swamped with requests and delays were observed in the review of non-COVID related clinical trial submissions.”
Vaccine support
The pandemics has also prompted the EMA to support efforts to develop SARS-CoV-2 vaccines and medical countermeasures for COVID-19.
For example, in April (4) the EMA established a COVID-19 taskforce to co-ordinate response to the pandemic. According to its mandate (5), the taskforce aims to identify promising vaccines and treatments, provide support for trials and foster cooperation between industry, regulators and international organisations.
These efforts will continue, according to Romero: “EMA is fully mobilised to support the development and marketing authorisation of safe, effective and high-quality COVID-19 vaccines.
“The Agency has put in place rapid review procedures to deliver assessments of high-quality applications from sponsors in the shortest possible timeframes while ensuring robust scientific opinions.”
Romero cites the provision of scientific advice as an example, explaining the agency helps with the design of studies needed to determine the safety, efficacy and quality of treatments and vaccines against COVID-19.
She adds that, as of 30 July 2020, the EMA has been in discussion with the developers of 38 potential vaccines and 154 potential COVID-19 treatments. These include immunomodulators, antivirals and hyperimmune serums.
The agency has also finalised 17 scientific advice procedures to provide developers with direction on the most appropriate methods and study designs for potential COVID-19 medicines. A further 15 such procedures are ongoing.
Industry response
“So far we have not received any application for Marketing Authorisation evaluation of a vaccine,” says Romero. “However, EMA encourages developers of potential vaccines or treatments for COVID-19 to contact EMA as soon as possible to discuss their strategy for evidence-generation.”
The EMA’s efforts have been welcomed by industry, according to Zhengxi Danard, who says the agency “has been extremely responsive by setting up quickly a COVID-19 Task Force to address the pharma industry requests.”
She cites the provision of “rapid scientific advice” as an example. “One of our clients is working on a candidate vaccine, and EMA has responded immediately to our request to engage with EMA experts to determine the best way forward to expedite the development of the product.
“In practice, they helped us define the endpoints for the pivotal study as well as the CMC developments which remain to be performed prior to Phase III.”
Help has also been provided at EU member state level, according to Danard: “The national competent authorities which are responsible for the review of clinical trial applications have followed suit by publishing guidelines and setting up expedited timelines for review of COVID-related clinical trials.”
However, the downside is that “dedicated resources for COVID specific topics to speed up the process, have impacted the other non COVID topics,” she adds.
Digital future
Romero says that at this stage, COVID-19 does not appear to have impacted drug industry submissions but warns “it is a bit premature” to comment on this: “EMA’s mid-year report for 2020 is currently being drafted and will be discussed by the Management Board at its 1 October meeting.
“However, what is clear so far is that the submission pipeline is healthy and marketing authorisation applications are not down in the first half of 2020 compared to 2019.”
The longer-term impact on drug development is unclear. However, what is certain is that the EMA will make greater use of digital resources.
“Obviously there are lessons that we can learn from the way we are working during the pandemic, and they will be integrated in our Regulatory Science Strategy going forward, but it is too early to say exactly how any changes might look,” continues Romero.
“The measures that we have put in place to deal with COVID-19 represent an extraordinary mobilisation of the network and given the resources required, this is not sustainable in the long term. We are doing this for COVID-19 medicines because there is such an unmet need, but we cannot do this all the time because it is very work intensive and at some stage resources will be exhausted.
“The pandemic has given all parties the opportunity to evaluate an increased use of digital technology in working practices. This experience can help to inform their greater adoption,” she says, adding “the process was already underway pre-pandemic but it’s now accelerated.”
Clinical considerations
The pandemic has also highlighted the benefits of regulatory flexibility, says Danard, who points to supply chain management and drug review processes as examples.
“The EU pharma regulations should also put in place mechanisms to expedite the development of international clinical studies to avoid the duplication of efforts among the different member states,” she says.
Danard also highlights the Voluntary Harmonisation Procedure for clinical trials - which will be formalized with the EU Clinical Trials Regulation implementation at the end of 2021 – as benefitting companies conducting trials during health emergencies.
“It will centralize the clinical trial approval process,” she says. “The focus however is more on harmonization and consistency of decisions rather than on shorter timelines. We have also to notice that ‘remote’ activity will be encouraged, and decisions about remove consultation, patient management out of hospital will grow.”
References:
1. https://www.karger.com/Article/FullText/508448
2. https://ec.europa.eu/health/sites/health/files/human-use/docs/guidance_regulatory_covid19_en.pdf
Related News
-
News PSCI Welcomes Delpharm, Samsung Biologics, and Suven as First Supplier Partners
The pharmaceutical industry continues to evolve with an increasing focus on responsible sourcing, sustainability, and collaboration across the supply chain. Under a new model to recognise suppliers within the pharmaceutical and healthcare industry that... -
News Drug prices agreed upon as part of the US Inflation Reduction Act
The Inflation Reduction Act brought into constitution by the Biden administation in 2022, which proposed a drug price negotiation between the government and pharmaceutical companies, has reached it's first agreement. -
News Eisai Alzheimer’s drug authorised in UK but still faces obstacles
In partnership with BioArctic AB, pharmaceutical company Eisai has been granted Marketing Authorisation by the Medicines and Healthcare products Regulatory Agency (MHRA) for its Alzheimer’s disease drug product Leqembi. -
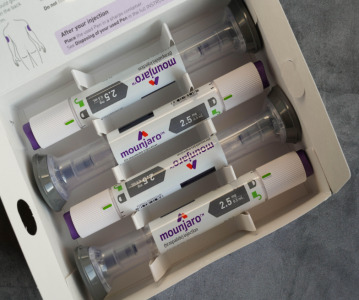
News Eli Lilly's weight loss drugs removed from the FDA's shortage list
The US FDA have recently updated their drug shortage list. The recently released list shows that all dosage forms of Eli Lilly's weight-loss drug Zepbound and their diabetes drug Mounjaro are now available. -
News Global advancements in the diagnosis and treatment of rare diseases: Rare Disease Day 2024
Rare Diseases Day is celebrated on the 29th February 2024 and represents the plight of rare disease patients to gain diagnosis and access to suitable treatment. -
News Pharmaceutical industry supports COP28 health stance in joint statement
As COP28 takes place over this week in Dubai, UAE, several bodies in the pharmaceutical and health industries have come together to announce support of key movements in sustainability in the sector, and to recognise sustainability as a health issue.&nb... -
News Biden backs Cold-War measures to shore-up medical supply chains
In a recent strategy to combat rising inflation and the cost of living crisis, President Joe Biden has invoked a Cold War-era act to increase investment in a selection of medicines and supplies. -
News CPHI Podcast Series: What does the changing US Pharma market mean for industry and patients alike?
In this week's episode of the CPHI Podcast Series Lucy Chard, Digital Editor for CPHI Online is joined by James Manser to discuss the political and market changes in the US pharma field.
Position your company at the heart of the global Pharma industry with a CPHI Online membership
-
Your products and solutions visible to thousands of visitors within the largest Pharma marketplace
-
Generate high-quality, engaged leads for your business, all year round
-
Promote your business as the industry’s thought-leader by hosting your reports, brochures and videos within your profile
-
Your company’s profile boosted at all participating CPHI events
-
An easy-to-use platform with a detailed dashboard showing your leads and performance


.png)