Researchers at the doorstep of stem cell therapies for MS, other myelin disorders
The potential to replenish populations of cells destroyed by disease was seen by many as the next medical revolution.
When the era of regenerative medicine dawned more than three decades ago, the potential to replenish populations of cells destroyed by disease was seen by many as the next medical revolution. However, what followed turned out not to be a sprint to the clinic, but rather a long tedious slog carried out in labs across the globe required to master the complexity of stem cells and then pair their capabilities and attributes with specific diseases.
In a review article appearing in the journal Science, University of Rochester Medical Center scientists Steve Goldman, M.D., Ph.D., Maiken Nedergaard, Ph.D., and Martha Windrem, Ph.D., contend that researchers are now on the threshold of human application of stem cell therapies for a class of neurological diseases known as myelin disorders – a long list of diseases that include conditions such as multiple sclerosis, white matter stroke, cerebral palsy, certain dementias, and rare but fatal childhood disorders called pediatric leukodystrophies.
"Stem cell biology has progressed in many ways over the last decade, and many potential opportunities for clinical translation have arisen," said Goldman. "In particular, for diseases of the central nervous system, which have proven difficult to treat because of the brain's great cellular complexity, we postulated that the simplest cell types might provide us the best opportunities for cell therapy."
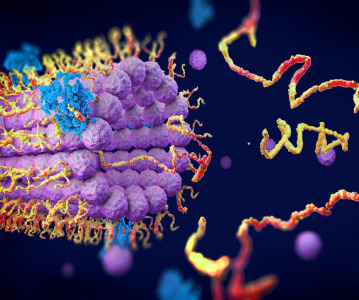
The common factor in myelin disorders is a cell called the oligodendrocyte. These cells arise, or are created, by another cell found in the central nervous system called the glial progenitor cell. Both oligodendrocytes and their "sister cells" - called astrocytes - share this same parent and serve critical support functions in the central nervous systems.
Oligodendrocytes produce myelin, a fatty substance that insulates the fibrous connections between nerve cells that are responsible for transmitting signals throughout the body. When myelin-producing cells are lost or damaged in conditions such as multiple sclerosis and spinal cord injury, signals traveling between nerves are weakened or even lost. Astrocytes also play an essential role in the brain. Long overlooked and underappreciated, it is now understood that astrocytes are critical to the health and signaling function of oligodendrocytes as well as neurons.
Glial progenitor cells and their offspring represent a promising target for stem cell therapies, because - unlike other cells
in the central nervous system - they are relatively homogeneous and more readily manipulated and transplanted. In the case of oligodendrocytes, multiple animal studies have shown that, once transplanted, these cells will disperse and begin to repair or "remyelinate" damaged areas.
"Glial cell dysfunction accounts for a broad spectrum of diseases, some of which - like the white matter degeneration of aging - are far more prevalent than we previously realized," said Goldman. "Yet glial progenitor cells are relatively easy to work with, especially since we don't have to worry about re-establishing precise point to point connections as we must with neurons. This gives us hope that we may begin to treat diseases of glia by direct transplantation of competent progenitor cells."
Scientists have reached this point, according to the authors, because of a number of key advances. Better imaging technologies - namely advanced MRI scanners - now provide greater insight and clarity into the specific damage caused in the central nervous system by myelin disorders. These technologies also enable scientists to precisely follow the results of their work.
Even more importantly, researchers have overcome numerous obstacles and made significant strides in their ability to manipulate and handle these cells. Goldman's lab in particular has been a pioneer in understanding the precise chemical signals necessary to coax stem cells into making glial progenitor cells, as well as those needed to "instruct" these cells to make oligodendrocytes or astrocytes. His lab has been able to produce these cells from a number of different sources – including "reprogramming" skin cells, a technology that has the advantage of genetically matching transplanted cells to the donor. They have also developed techniques to sort these cells based on unique identifying markers, a critical step that ensures the purity of the cells used in transplantation, lowering the risk for tumor formation.
Nedergaard's lab has studied the integration of these cells into existing neural networks, and well as in imaging their structure and function in the adult nervous system. Together, the two labs have developed models of both human neural activity and disease based on animals transplanted with glial progenitor cells, which will enable human neural cells to be evaluated in the context of the live adult brain – as opposed to a test tube. This work has already opened new avenues in both modeling and potentially treating human glial disease.
All of these advances, contend the authors, have accelerated research to the point where human studies for myelin disorders are close at hand. For instance, diseases such as multiple sclerosis, which benefit from a new generation of stabilizing anti-inflammatory drugs, may be an especially appealing target for progenitor-based cell therapies which could repair the now permanent and untreatable damage to the central nervous system that occurs in the disease. Similarly, the authors point to a number of the childhood diseases of white matter that now appear ripe for cell-based treatment.
"We have developed a tremendous amount of information about these cells and how to produce them," said Goldman. "We understand the different cell populations, their genetic profiles, and how they behave in culture and in a variety of animal models. We also have better understanding of the disease target environments than ever before, and have the radiographic technologies to follow how patients do after transplantation. Moving into clinical trials for myelin disorders is really just a question of resources at this point."
Related News
-
News A Day in the Life of a Start-Up Founder and CEO
At CPHI we work to support Start-Up companies in the pharmaceutical industry and recognise the expertise and innovative angles they bring to the field. Through our Start-Up Programme we have gotten to know some of these leaders, and in this Day in the ... -
News Biopharmaceutical manufacturing boost part of new UK government budget
In their national budget announced by the UK Labour Party, biopharmaceutical production and manufacturing are set to receive a significant boost in capital grants through the Life Sciences Innovative Manufacturing Fund (LSIMF). -
News CPHI Podcast Series: The power of proteins in antibody drug development
In the latest episode of the CPHI Podcast Series, Lucy Chard is joined by Thomas Cornell from Abzena to discuss protein engineering for drug design and development. -
News Amgen sues Samsung biologics unit over biosimilar for bone disease
Samsung Bioepis, the biologics unit of Samsung, has been issued a lawsuit brought forth by Amgen over proposed biosimilars of Amgen’s bone drugs Prolia and Xgeva. -
News CPHI Podcast Series: Why we need to consider women in clinical trials
The latest episode of the CPHI Podcast Series with Lucy Chard covers women's health, specifically women's representation in clinical trials, the associated bias, and the impacts on health for this population. -
News US FDA does not approve MDMA therapy for PTSD, requests more data
The MDMA-based therapeutic developed by Lykos Therapeutics, a California-based Public Benefit Corporation (PBC), has been reviewed and unapproved by the US FDA. The regulator has requested additional phase III trial data for further safety and efficacy... -
News Novartis and Viatris latest facing lawsuit over HeLa cell misuse
Global pharmaceutical companies Novartis and Viatris are the latest hit with a lawsuit claim pertaining to alleged misuse of the ‘HeLa’ cell line from the estate of woman whose cancerous tissue cells were taken without consent. -
News Sanofi invests billions into Frankfurt insulin production site
French pharmaceutical company Sanofi have announced an investment of EUR1.3 billion at their existing BioCampus site in Frankfurt am Main for the expansion of insulin production.
Position your company at the heart of the global Pharma industry with a CPHI Online membership
-
Your products and solutions visible to thousands of visitors within the largest Pharma marketplace
-
Generate high-quality, engaged leads for your business, all year round
-
Promote your business as the industry’s thought-leader by hosting your reports, brochures and videos within your profile
-
Your company’s profile boosted at all participating CPHI events
-
An easy-to-use platform with a detailed dashboard showing your leads and performance


.png)

.png)
.png)
.png)